01 March, 2024
Cystatin C (CysC) is a remarkable protein with many roles. It is an early marker of acute kidney injury (AKI), a superior marker of kidney transplant function and transplant failure, and offers a more accurate measurement of liver cirrhosis. Research has suggested cystatin C’s potential role in the diagnosis and prognosis of cardiovascular (CVD) risk and oncology 1.
Chronic Kidney Disease
Prevalence
Chronic kidney disease (CKD) is a serious, progressive condition characterised by a decrease in kidney function. CKD is a substantial burden globally, affecting >10% of the global population (>800m individuals), with the majority undiagnosed. It affects various demographic groups, including: older individuals, women, racial minorities, and those with hypertension or diabetes. This burden is particularly pronounced in low- and middle-income countries, which often lack the resources to effectively manage its consequences. CKD has become a leading cause of mortality globally, experiencing an increase in associated deaths over the past two decades, making it one of the most prominent causes of death and suffering in the 21st century 2.
The rise in risk factors such as obesity and diabetes has contributed to the increasing prevalence of CKD. While mortality rates in patients with end-stage kidney disease (ESKD) have seen a decline, CKD remains a significant contributor to global mortality according to the Global Burden of Disease (GBD) studies. As such, there is a pressing need for improved identification, monitoring, and treatment of CKD, along with the implementation of preventative and therapeutic measures on a global scale 2.
Efforts to address CKD should encompass not only treatment but also prevention strategies, given its association with modifiable risk factors such as obesity and diabetes. Additionally, greater attention should be directed towards understanding CKD epidemiology in various populations, including paediatric patients, and assessing its impact on clinical outcomes such as CVD. By addressing these aspects comprehensively, healthcare systems can better mitigate the adverse effects of CKD and improve patient outcome worldwide 2.
Economic Burden
CKD presents a significant economic burden globally, especially as it progresses to kidney failure. The necessity for resource-intensive kidney replacement therapy (FRT), which includes dialysis or kidney transplantation, imposes substantial healthcare costs and societal burdens. Additionally, advanced CKD is associated with an elevated risk of cardiovascular disease (CVD), including: heart failure, myocardial infarction and stroke, further escalating healthcare resource utilisation and economic strain. This dual impact on both healthcare costs and societal burdens underscores the importance of effective management and prevention strategies for CKD. Table 1 below highlights the costs associated with increased disease progression and severity, with further costs associated with regards to complications 3.
|
Table 1: Economic Burden of CKD & Associated Complications 3
|
|
Disease State / Intervention
|
Cost
|
|
Acute Kidney Injury (AKI)
|
$5,975
|
|
Stage G3a
|
$3,060
|
|
Haemodialysis
|
$57,334
|
|
Peritoneal dialysis
|
$49,490
|
|
Transplant
|
$75,326
|
|
Myocardial infarction
|
$18,294
|
|
Heart failure
|
$8,463
|
|
Stroke
|
$10,168
|
Early detection and intervention are crucial in mitigating the devastating effects of CKD. Implementing strategies for early testing, particularly in high-risk populations such as those with diabetes, hypertension, and obesity, can help identify CKD at its earliest stages when interventions are most effective 3.
CKD Classification
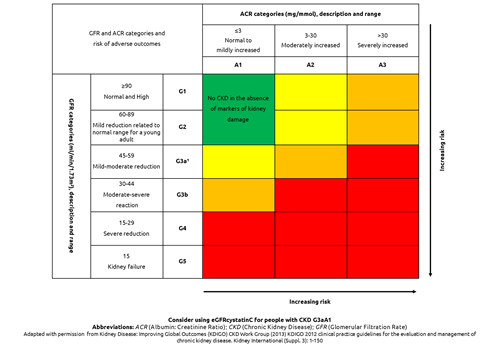
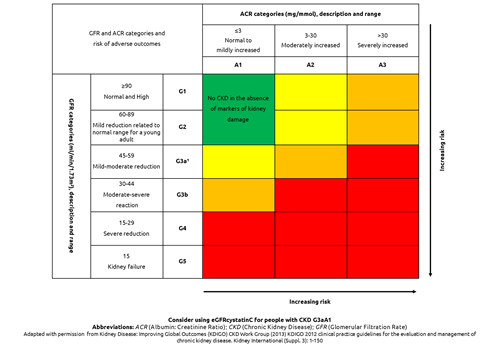
The modern classification for CKD is based on a combination of estimated glomerular rate (eGFR) and urinary albumin:creatinine rate (ACR) as highlighted in Figure 1 4.
Both increased ACR and decreased GFR are independently associated with an increased risk of adverse outcomes such as cardiovascular events (CVE), kidney failure, and mortality. When both increased ACR and decreased GFR are present in combination, the risk of adverse outcomes is multiplied, indicating a more severe form of kidney disease. This highlights the importance of considering both markers in the assessment and management of CKD patients 4.
Figure 1: Classification of CKD using eGFR and urinary ACR categories 4

Cystatin C is a further marker of renal function that can be utilised in eGFR, particularly in situations where eGFR based on serum creatinine may be less accurate. It is worth noting that CysC is less influenced by factors such as muscle mass, which can affect serum creatinine levels. Therefore, CysC may provide a more accurate assessment of renal function in certain populations, especially those with borderline renal function or individuals without evidence of proteinuria 4.
The KDIGO CKD Work Group recommends considering additional tests like CysC for confirmatory testing in specific circumstances where eGFR based on serum creatinine might not be reliable. However, it is important to acknowledge that CysC is not as widely available in clinical practice as serum creatinine testing and its use may depend on local laboratory availability and practices 4.
Aetiology of Cystatin C
Cystatin C is a 13kDa protein encoded by the CST3 gene. It is a non-glycosylated, basic protein found in all nucleated cells. CysC functions as a potent inhibitor of lysosomal proteinases and extracellular inhibitors of cysteine proteases, playing a significant role in regulating various cellular processes, including: protein degradation, apoptosis (programmed cell death), and immune response regulation1.
One crucial aspect of CysC is its role as a measure of renal function, specifically filtration. It is generated at a relatively constant rate and undergoes processes such as filtration, reabsorption, and catabolism in the proximal tubule of the nephron. As CysC is not influenced by sex, age or muscle mass, it is considered to be a more accurate marker of renal function. As CysC is less affected by external factors compared to creatinine, it is considered by many healthcare professionals to be a more reliable marker for estimating GFR, the key indicator of renal function. Consequently, CysC measurements are often used in conjunction with creatinine measurements to provide a more accurate assessment of renal health1.
CysC has also been implicated in various other physiological processes and pathological conditions, including cardiovascular disease, neurodegenerative disorders, and cancer, highlighting cystatin C’s broader significance in human health beyond renal function assessment 1.
A Biomarker of Renal Dysfunction
Several studies support the utility of cystatin C as a biomarker of renal dysfunction.
- Cystatin C predicts long term mortality better than creatinine in a nationwide study of intensive care patients (2021) 5
A Swedish study prospectively evaluated 22,488 intensive care (ICU) patients at three hospitals in Sweden between 2004 and 2015 with a medium follow-up of 5.1years. The study investigated the predictive value of eGFR using different equations based on creatinine, cystatin C, and a combination of both, in critically ill patients.
The findings suggested that using a cystatin C-based equation for estimating GFR may provide better risk prediction for mortality in critically ill patients compared to using creatinine-based equations. Therefore, the study supports the use of CysC as a biomarker for eGFR in this patient population.
- Serum cystatin C as a biomarker for early diabetic kidney disease and dyslipidemia in young type 1 diabetic patients (2022) 6
A Lithuanian study prospectively evaluated 779 subjects with a median age of 16.2 years, with a medium diabetes duration of 5.3 years to investigate the clinical significance of serum cystatin C in the early detection of renal injury and its association with dyslipidaemia in young patients with type 1 diabetes (T1D).
The study concluded that cystatin C can serve as an additional biomarker for the early detection of renal injury in young patients with T1D. The findings also indicate an association between cystatin C levels and both glycaemic control (HbA1c) and HDL cholesterol levels.
- Circulating cystatin C is an independent risk marker for cardiovascular outcomes, development of renal impairment, and long-term mortality in patients with stable coronary heart disease: The LIPID Study (2022) 7
An American study of 7,863 patients with a follow-up of 6,106 patients in the LIPID (Long-Term Intervention with Pravastatin in Ischemic Disease) study, who had previous acute coronary syndrome to determine the association between circulating levels of cystatin C and various health outcomes in this patient population.
In summary, the study highlights CysC as a robust and independent predictor of major cardiovascular events, development of CKD, and both cardiovascular and all-cause mortality in patients with stable coronary heart disease (CHD). Its prognostic value extends beyond traditional markers of renal function and underscores its utility in risk stratification and clinical management of individuals with CHD.
- Assessment of cystatin C level for risk stratification in adults with chronic kidney disease (2022) 8
A UK population-based cohort study prospectively evaluated 428,402 patients with participants recruited between 2006-2010 with a median follow-up of 11.5 years. Participants were stratified into older (65-73 years) and younger (<65 years) groups.
The study highlights the importance of assessing renal function using cystatin C levels in addition to serum creatinine for more accurate risk stratification in individuals with mild CKD. Incorporating cystatin C measurement into clinical practice may enhance the identification of individuals at higher risk of CVD and mortality, ultimately guiding clinical decision-making and improving patient outcomes.
Conclusion
In conclusion, unlike creatinine, cystatin C is less influenced by factors such as muscle mass, age, sex and diet. This makes it particularly useful in populations where these factors may vary significantly, such as in children, the elderly, and individuals with muscle wasting conditions. Additionally, CysC has been shown to be a sensitive marker for the detection of early stage renal dysfunction, often before changes in serum creatinine become apparent. Therefore, CysC is increasingly being utilised alongside creatinine for a more accurate assessment of renal function, especially in individuals with conditions like diabetes, CKD and CVD. Overall, CysC serves as a valuable biomarker for eGFR and the detection of early kidney dysfunction, offering clinicians additional insights into a patient’s renal health beyond traditional markers like creatinine.
Fortress Cystatin C Solutions
Quote our promotional code ‘CYSC24’ for a discount on Cystatin C products.
References
- Fernando S, Polkinghorne KR. Cystatin C: not just a marker of kidney function. Brazilian Journal of Nephrology 2020; 42(1). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7213924/ (accessed 14 February 2024).
- Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney International Supplements 2022; 12(1). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9073222/ (accessed 14 February 2024).
- Jha V, Al-Ghamdi SMG, Li G, Wu MS, Stafylas P, et al. Global Economic Burden Associated with Chronic Kidney Disease: A Pragmatic Review of Medical Costs for the Inside CKD Research Programme. Advances in Therapy 2023; 40. https://link.springer.com/article/10.1007/s12325-023-02608-9 (accessed 27 February 2024).
- National Institute of Care Excellence. What initial investigations should I arrange?. https://cks.nice.org.uk/topics/chronic-kidney-disease/diagnosis/initial-investigations/ (accessed 27 February 2024).
- Helmersson-Karlqvist J, Lipcsey M, Ärnlöv J, Bell M, Ravn B, et al. Cystatin C predicts long term mortality better than creatinine in a nationwide study of intensive care patients. Scientific Reports 2021; 11(5882). https://www.nature.com/articles/s41598-021-85370-8 (accessed 28 February 2024).
- Stankute I, Radzevičienė L, Monstaviciene A, Dobrovolskiene R, Danyte E, et al. Serum Cystatin C as a Biomarker for Early Diabetic Kidney Disease and Dyslipidemia in Young Type 1 Diabetes Patients. Medicina 2022; 58(2). https://www.mdpi.com/1648-9144/58/2/218 (accessed 28 February 2024).
- West M, Kirby A, Stewart RA, Blankenberg S, Sullivan D, et al. Circulating Cystatin C Is an Independent Risk Marker for Cardiovascular Outcomes, Development of Renal Impairment, and Long‐Term Mortality in Patients With Stable Coronary Heart Disease: The LIPID Study. Journal of the American Heart Association (JAMA) 2022; 11(5). https://www.ahajournals.org/doi/10.1161/JAHA.121.020745 (accessed 27 February 2024).
- Lees JS, Rutherford E, Stevens KI, Chen DC, Scherzer R, et al. Assessment of Cystatin C Level for Risk Stratification in Adults With Chronic Kidney Disease. Journal of the American Medical Association https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2797627 (accessed 28 February 2024).